Treatment
Glaucoma Treatment
Get an appointment with an ophthalmologist to treat your glaucoma in as quickly as three days. No referral needed.
Glaucoma cannot yet be cured, and the treatments currently in use aim to reduce intraocular pressure (IOP) in order to prevent any further damage to the optical nerve.
Any vision loss caused by glaucoma is irreversible; however, with consistent treatment, and regular and comprehensive eye examinations, it’s possible to stop and prevent further loss of vision from a damaged optical nerve.
Regular eye examinations that include IOP measurements are essential to detect reduced or impaired vision as early as possible. If left undetected and untreated, glaucoma can lead to irreversible blindness.
Treatment types
Glaucoma treatment offered at Vision Pros Ophthalmology Clinic includes the following:
- Eye drops, gels and medications
- Laser treatment
- Surgery
- Implants
Take a closer look at the medical, laser, and surgical procedures available to treat glaucoma.


Eye drops, gels and medications
Eye drops, gels, and medications are some of the first and second-line treatment options for glaucoma and include the following:
- Alpha-adrenergic agonists
- Beta-blockers
- Carbonic anhydrase inhibitors
- Miotics or cholinergic agents
- Prostaglandin analogs
- Rho kinase inhibitors
Alpha-adrenergic agonists eyedrops reduce the amount of aqueous fluid that is produced by the eye and allow the fluid to escape the eye, reducing the intraocular pressure (IOP).
Beta-blockers eyedrops also work to reduce IOP by reducing the amount of aqueous fluid produced by the ciliary body of the eye.
Carbonic anhydrase inhibitors are an oral glaucoma medication that also lowers eye pressure by improving your eye’s ability to drain excess aqueous fluid through the eye’s trabecular meshwork (drainage system). Carbonic anhydrase inhibitors are prescribed in cases of uncontrollable high pressure that doesn’t respond to eye drops or when there’s a high risk of rapid vision loss.
Miotics or cholinergic agents help to reduce IOP by improving the flow of aqueous fluid from your eye, and they may also help to relieve dry eyes.
Prostaglandin analogs are arguably the most effective at lowering eye pressure, with the fewest side effects from the eye drops, gels, and medication used to treat glaucoma.
Rho kinase inhibitors or rock inhibitors are some of the latest innovations in glaucoma treatment and reduce eye pressure by changing the structure of the eye’s drainage system to improve the flow of aqueous fluid.
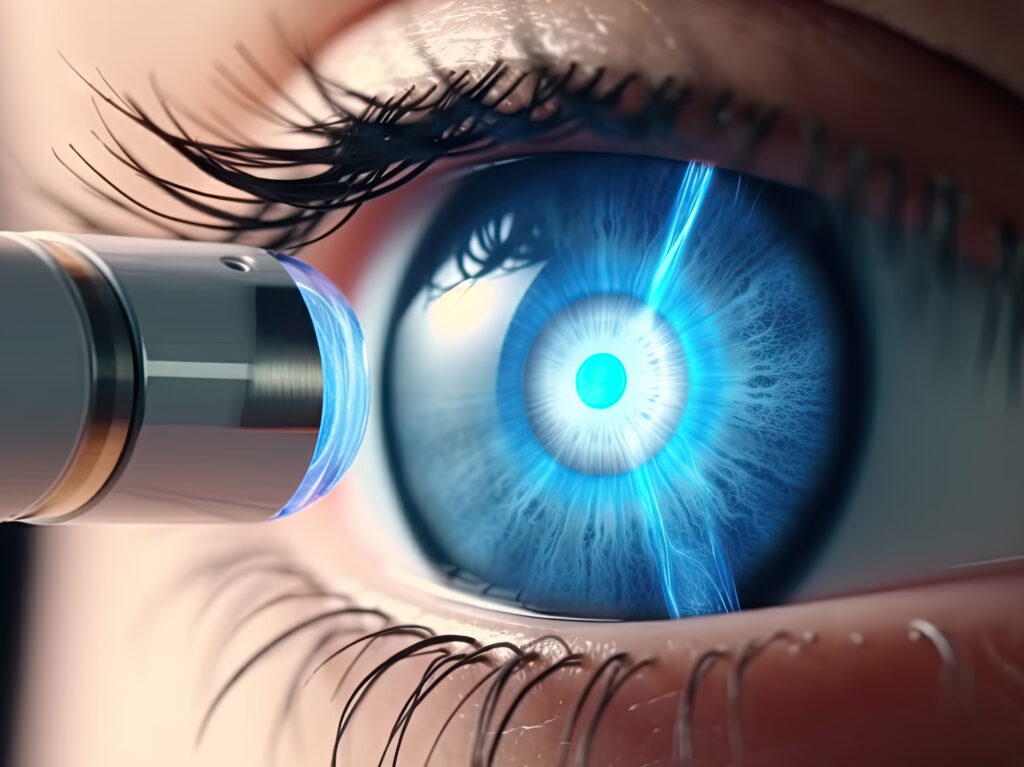
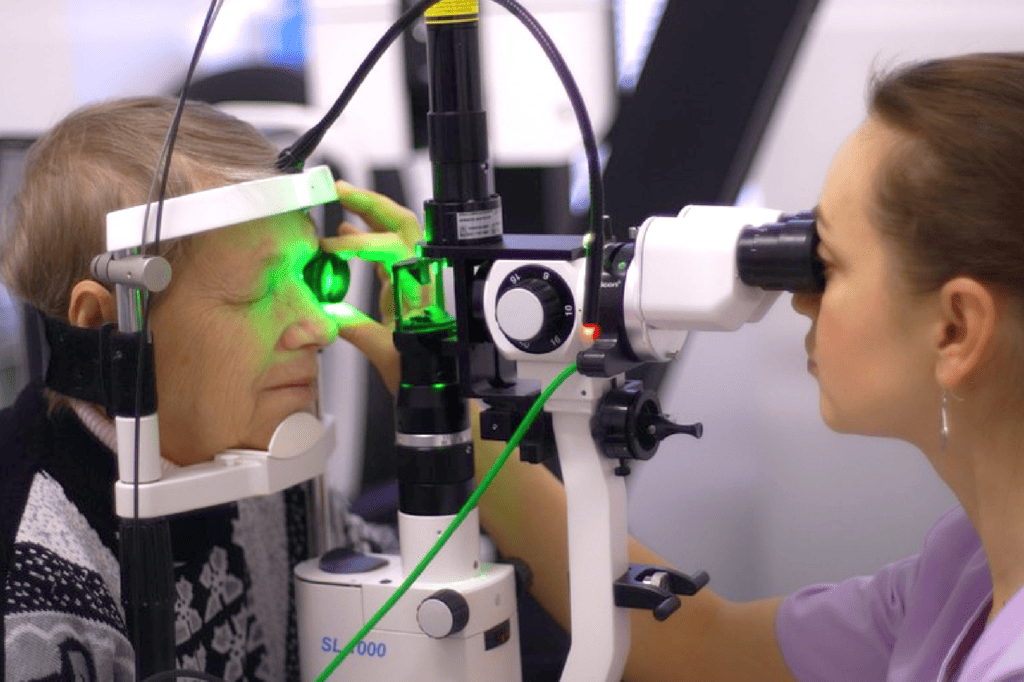
Laser treatment
Most laser treatments for glaucoma lower intraocular pressure by changing the trabecular meshwork or drainage system of the eye.
In the case of glaucoma, your eye’s trabecular meshwork may function less effectively at draining the aqueous fluid produced inside your eye.
If the aqueous fluid doesn’t drain and flow out of your eye, the pressure inside your eye may rise and damage your optical nerve, which may lead to permanent vision loss.
Vision Pros offers the following laser procedures to treat glaucoma:
- Trabeculoplasty
- Iridotomy
- Iridoplasty
- Cyclodestructive procedures
Trabeculoplasty
The main types of trabeculoplasty performed at Vision Pros to treat glaucoma are selective laser trabeculoplasty (SLT), argon laser trabeculoplasty (ALT), and micropulse laser trabeculoplasty (MLT).
Argon laser trabeculoplasty is the earlier form of glaucoma laser treatment.
While SLT can be performed to treat glaucoma even if ALT has already taken place, the reverse isn’t true.
Today, selective laser trabeculoplasty is recommended over ALT because the resulting microscopic scarring from ALT may limit further surgical options.
Micropulse laser trabeculoplasty is essentially a newer version of SLT that aims to reduce scarring and postoperative intraocular pressure (the internal eye pressure increase caused by inflammation of the eye tissue after surgery).
Iridotomy
During an iridotomy, the ophthalmologist creates a single opening in the iris of the eye to allow better drainage of the aqueous fluid and relief of the intraocular pressure.
If you’ve already been diagnosed with chronic narrow-angle glaucoma, laser peripheral iridotomy can be recommended in order to mitigate the risk of acute closed-angle glaucoma, which is an emergency.
Iridoplasty
An iridoplasty may be the next step should an iridotomy not reduce internal eye pressure enough to prevent optical nerve damage. During an iridoplasty, an ophthalmologist uses laser to shrink your iris and widen the drainage angle of your eye and improve the flow of aqueous fluid out of the eye cavity.
Cyclodestructive procedures
Your ophthalmologist may suggest a cyclodestructive procedure to treat a case of refractory glaucoma that hasn’t responded to other treatment methods.
Cyclophotocoagulation (CPC) is the most commonly performed cyclodestructive glaucoma treatment procedure.
During CPC, a laser is directed at the ciliary body (the part of your eye responsible for producing aqueous fluid) to reduce the production of aqueous fluid and lower the intraocular pressure.
Other types of cyclodestructive glaucoma treatment include endoscopic cyclophotocoagulation (ECP), micropulse transscleral cyclophotocoagulation, and cycloablation via ultrasound.
Surgery
While laser technology is widely used to treat glaucoma, non-laser surgery is still very much used to lower intraocular pressure.
Vision Pros ophthalmologists hold vast experience in the following surgical procedures:
- Filtering surgery
- Trabeculectomy
- Peripheral iridectomy
- Canaloplasty
- Goniotomy


Filtering surgery
Filtering or conventional surgery to treat glaucoma consists of creating new pathways for the aqueous fluid to drain more effectively through the trabecular meshwork.
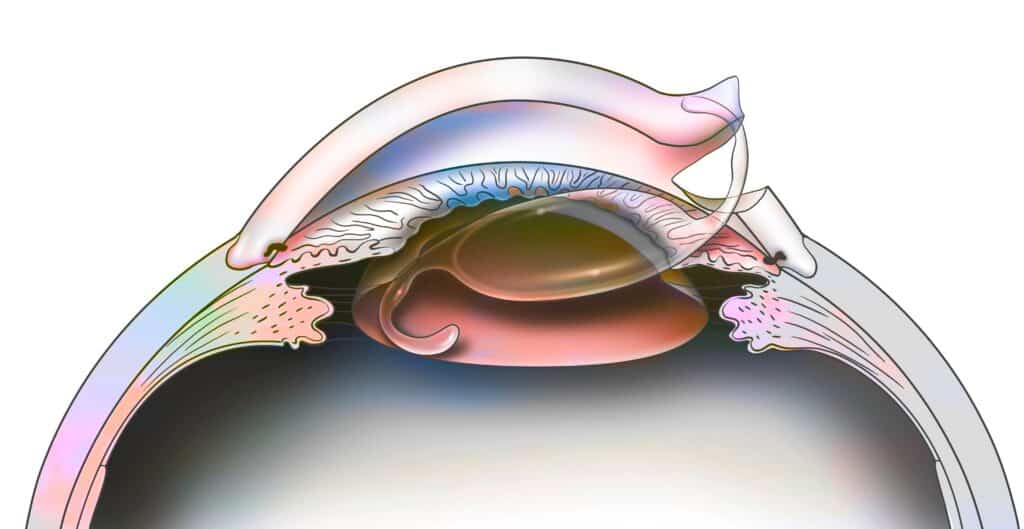
Trabeculectomy
During a trabeculectomy, the ophthalmologist removes a piece of the trabecular meshwork in order to create a new opening for draining aqueous fluid and lowering eye pressure.
Peripheral iridectomy
A peripheral iridectomy entails removing a thin portion of the iris so that aqueous fluid can drain out of the eye easily.
Canaloplasty
During a canaloplasty, the ophthalmologist inserts a microcatheter inside Schlemm’s canal, the passage through which aqueous fluid drains out of the eye. By expanding this canal, intraocular pressure can be reduced enough to prevent further damage to the optical nerve.
Goniotomy
Goniotomy is a minimally invasive glaucoma surgery almost exclusively used to treat congenital glaucoma in infants and children.
During infant goniotomy, the ophthalmologist makes a small incision in the cornea and remove a portion of the trabecular meshwork so that aqueous fluid can drain out of the eye and lower IOP.
Goniotomy isn’t usually recommended to treat adult glaucoma because the resulting scarring of the cornea may worsen aqueous fluid drainage and higher intraocular pressure.
Implants
An ophthalmologist may recommend two types of implants to lower eye pressure and improve the flow of fluid out of your eye: drug-delivery implants and drainage implant devices.

Drug-delivery implants
Prostaglandin analog implants are cutting-edge biodegradable drug-delivery technology that shows promising results in maintaining intraocular pressure and preventing further damage to the optical nerve in cases of glaucoma.
Drainage implant devices
Drainage implant devices like shunts and tubes may help enlarge the trabecular meshwork in your eye to allow more aqueous fluid to drain out of the eye and relieve the pressure on the optical nerve.
Note that you can access additional in-hospital glaucoma surgical procedures performed via the Vision Pros network of hospitals throughout Montreal and Quebec.
Preparing for glaucoma treatment
The Vision Pros team will guide and support you as you prepare for glaucoma treatment, whether you’re prescribed medication or are scheduled for conventional or laser surgery.

Eye drops, gels and medications
You might need to take more than one type of eye drop, gel, or medication at a time to lower your eye pressure and improve the flow of aqueous fluid.
Your Vision Pros ophthalmologist will explain when and how to take each of your glaucoma medications so that they’re most effective at reducing your eye pressure with minimal side effects.
Life can get busy, and you might forget to take your glaucoma medication as prescribed, so try using an app or calendar to keep track of your medication schedule.
You can also use an eye drops applicator to reduce the amount of medication that enters other parts of the body through the tear ducts, so you don’t waste any medication and avoid red eyes, skin discoloration, and other unwanted systemic side effects.
Note that eye drops, gels, and medications may also be prescribed in preparation for laser or traditional glaucoma surgery.
Laser treatment
In preparation for glaucoma laser treatment, your Vision Pros ophthalmologist may prescribe eye drops or medication, and it’s essential you take your medication as and when directed for the best results possible.
Here are a few tips to prepare for glaucoma laser surgery:
- Remove your contact lenses or glasses and any jewellery near the eye area.
- Keep your eyes and face clean and free from make-up, moisturizers, creams or lotions.
- Wear comfortable clothing; ideally a shirt or top that’s easy to unbutton or unzip without making contact with your eyes.
- Avoid food and drink prior to the laser treatment if directed by the ophthalmologist.
- Avoid alcohol at least 48 hours before treatment to reduce the risk of complications after laser surgery.
- If you smoke, it’s best to stop well before the laser treatment, as smoking can interfere with the healing process.
- You may also need to stop taking certain chronic medications like blood thinners a few days or more before your treatment.
Surgery
Similarly to laser surgery, you might be prescribed eye drops or medication before undergoing glaucoma surgeries like a trabeculectomy or a canaloplasty.
Here’s what else you might expect before glaucoma surgery:
- A pre-operative evaluation will take place a few weeks before your surgery is scheduled to identify issues such as heart problems.
- You may be asked to stop taking chronic medications that may lead to complications during surgery.
- You’ll need to avoid water and food the night before your glaucoma surgery.
- Remove your contact lenses or glasses and any jewelry near the eye area.
- Keep your eyes and face clean and free from make-up, moisturizers, creams or lotions.
- Avoid alcohol at least 48 hours before treatment to reduce the risk of complications after laser surgery.
- If you smoke, it’s best to stop well before the laser treatment, as smoking can interfere with the healing process.
Implants
As implants are inserted in your eye using minimally invasive glaucoma surgery, you should prepare for glaucoma implant surgery the same way you would for filtering surgery or an iridectomy.

What happens during treatment?
Medication and laser treatment for glaucoma are fairly straightforward procedures, while glaucoma surgery and implants may require a slightly more involved illustration.
Find out what happens during the various glaucoma treatment options offered at Vision Pros.
Eye drops, gels and medications
Applying glaucoma eye drops, gels, and medication follows these simple steps:
- Wash your hands.
- Gather the eye drops, gel, and medication you need, as well as some cotton, tissue paper or paper towel, and alcohol swabs.
- Use an alcohol swab to sterilize the medication’s bottle cap.
- Let the alcohol evaporate off the cap and your fingers so you don’t accidentally sting your eye.
- Open the medication cap or stopper.
- If you have an eye drop applicator, place a drop of the medication on it.
- Tilt your head back and create a pouch by gently pulling your lower eyelid away from your eye.
- Apply the eye drop applicator to the eye or place one drop into the pouch created by your lower eyelid.
- Try not to blink, close your eye, and press a cotton ball or bunched-up tissue or paper towel between the corner of your eye and the bridge of your nose to block the tear duct.
- Hold for at least 30 seconds.
- Make sure to wipe any medication that’s spilt onto the skin around your eye.
- Repeat steps 6 to 11 on the other eye, if necessary.
- Dispose of the used cotton and paper, wash your hands and the eye drop applicator, and store your medication as directed by your ophthalmologist.
It’s important to effectively block your tear ducts after each eye drop application to avoid systemic side effects caused by the ingredients in your glaucoma medication
If you have more than one set of eye drops to apply, wait at least five minutes before each application.
If you apply one set of eye medication immediately after the previous one, you risk washing out the first eye drop application.
Finally, remember that It’s best to apply eye drops before gels and emulsions, as the latter can prevent drops from being properly absorbed by the eye.
Your Vision Pros ophthalmologist will explain when and how to take each of your glaucoma medications so that they’re most effective at reducing your eye pressure with minimal side effects.
Life can get busy, and you might forget to take your glaucoma medication as prescribed, so try using an app or calendar to keep track of your medication schedule.
You can also use an eye drops applicator to reduce the amount of medication that enters other parts of the body through the tear ducts, so you don’t waste any medication and avoid red eyes, skin discoloration, and other unwanted systemic side effects.
Note that eye drops, gels, and medications may also be prescribed in preparation for laser or traditional glaucoma surgery.
Laser treatment
Whether you’re undergoing a laser trabeculoplasty, iridotomy, iridoplasty, or a cyclodestructive procedure, you can expect a glaucoma laser treatment to follow these steps:
- The ophthalmologist will apply anesthetic medication in the form of eye drops to numb your eye.
- You’ll sit in front of a slit lamp used by the ophthalmologist to see clearly inside your eye.
- A face-holder may be necessary to keep your head still during the procedure.
- Next, a contact lens will be placed on your eye to direct the laser energy to the precise location of your eye that requires treatment.
- After the laser treatment, the ophthalmologist will apply eye drops or an ointment to reduce inflammation in your eye.
- The ophthalmologist will then measure your eye pressure.
- You’ll be allowed to rest for a short while in a recovery room before going home.
Surgery
On the day of your non-laser glaucoma surgery, the Vision Pros ophthalmology team will guide you through the following steps:
- Make sure to take any eye drops or medication as directed.
- You’ll receive anesthetic eye drops to numb your eye before surgery.
- You may also be given medication to keep you relaxed during surgery.
- In the case of a surgical procedure like canaloplasty, you’ll be under anesthesia.
- The ophthalmologist will use an eyelid holder to keep your eye open and proceed with the surgery.
- After the surgical procedure, self-dissolving stitches will be used to close the incisions.
- Eye drops or an ointment will be applied, and a bandage will be placed over your eye to prevent infection.
- The ophthalmologist will then measure your eye pressure, and you’ll be able to rest before going home.
- A metal or plastic shield may be recommended to protect your eye during recovery.
Implants
Drug-delivery implants and drainage implant devices for glaucoma are typically inserted via minimally invasive surgical procedures.
As such, minimally invasive glaucoma surgeries (MIGS) follow similar steps to more invasive surgeries such as iridectomy or canaloplasty:
- Make sure to take any eye drops or medication as directed on the day of surgery.
- You’ll receive anesthetic eye drops to numb your eye before surgery.
- You may also be given medication to keep you relaxed during surgery.
- The ophthalmologist will use an eyelid holder to keep your eye open and proceed with the surgery.
- After the surgical procedure, self-dissolving stitches will be used to close the incisions.
- Eye drops or an ointment will be applied, and a bandage will be placed over your eye to prevent infection.
- The ophthalmologist will then measure your eye pressure, and you’ll be able to rest before going home.
- A metal or plastic shield may be recommended to protect your eye during recovery.
Recovering from glaucoma treatment
Depending on the type of treatment you receive, recovering from conventional or laser glaucoma surgery should take a few days to a few weeks.
Follow-up treatment after glaucoma surgery typically requires the following:
- Make sure to attend every post-op appointment with your ophthalmologist.
- Take every medication as directed by your eye surgeon.
- Wear protective eyewear like eye shields and sunglasses, and avoid contact lenses until your surgeon clears them.
- Apply eye drops and medications according to the schedule prescribed by your ophthalmologist.
- You may experience painful and itchy eyes, but it’s important to avoid rubbing your eyes to prevent infection and damage to your eyes.
- Don’t drive until cleared by your eye doctor.
- Avoid bending too low, as it may worsen your eye pressure.
- Avoid activities that put a strain on your eyes, such as reading or lifting heavy objects, for a few weeks after glaucoma treatment or surgery.
Contact your ophthalmologist if you notice any of the following as they could be signs of infection:
- Pus or discharge from your eye
- Redness or swelling of your eye
- Fever

Why choose Vision Pros to treat your glaucoma?
- Experienced ophthalmology team of specialists with expertise in all areas of ophthalmology, optometry, and general eye care.
- Rapid access and referral to world-class comprehensive screening and cutting-edge treatment in a state-of-the-art ophthalmology clinic.
- Holistic, personal, and patient-centric approach to every aspect of eye care.
Schedule your comprehensive glaucoma examination today
- https://www.brightfocus.org/
- https://opto.ca/eye-health-library
- https://familydoctor.org/diseases-and-conditions/
- https://www.allaboutvision.com/
- https://opto.ca/eye-health-library/glaucoma
- https://occeyecare.ca/pages/Glaucoma
- https://youtu.be/Ul12Sud2Yos
- https://youtu.be/xisHasaahns
- https://youtu.be/QjmB_OdDrl4
- https://youtu.be/Nncc8dL_ThI
- https://youtu.be/yyR6QcS8kQQ
- https://youtu.be/EwsVmTOBZrc
- https://youtu.be/mc9GsvMlaCc
- https://youtu.be/I4f6RiBROYE
- https://youtu.be/LNfp3c1Wf0I
- https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD012223.pub2/full
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6267695/
- https://www.intechopen.com/chapters/80679
- https://www.ottawahospital.on.ca/en/documents/2017/01/ei-glaucoma-e.pdf/