Conditions
Diabetic retinopathy
Diabetic retinopathy has been identified by Fighting Blindness Canada (FBC) as one of the “big five” eye diseases affecting millions of Canadians, along with age-related macular degeneration, cataracts, glaucoma, and eye injuries.
What is diabetic retinopathy?
Diabetic retinopathy is an eye disease that may affect you if you’ve been diagnosed with diabetes.
Diabetic retinopathy usually progresses through 4 stages:
- Mild nonproliferative retinopathy
- Moderate nonproliferative retinopathy
- Severe nonproliferative retinopathy
- Proliferative diabetic retinopathy (PDR)
This eye condition affects blood vessels in the retina and may lead to vision loss if left untreated, as well as other diseases such as:
- Diabetic macular edema (DME)
- Neovascular glaucoma
- Tractional retinal detachment
Our Vision Pros specialists recommend a comprehensive dilated eye exam at least once a year, as you might not be aware of the initial symptoms of diabetic retinopathy.

What causes diabetic retinopathy?
Diabetic retinopathy can be caused by the following types of diabetes:
- Type 1 diabetes
- Type 2 diabetes
- Gestational diabetes, which develops during pregnancy
The longer you have diabetes, the higher your risk of developing diabetic retinopathy.
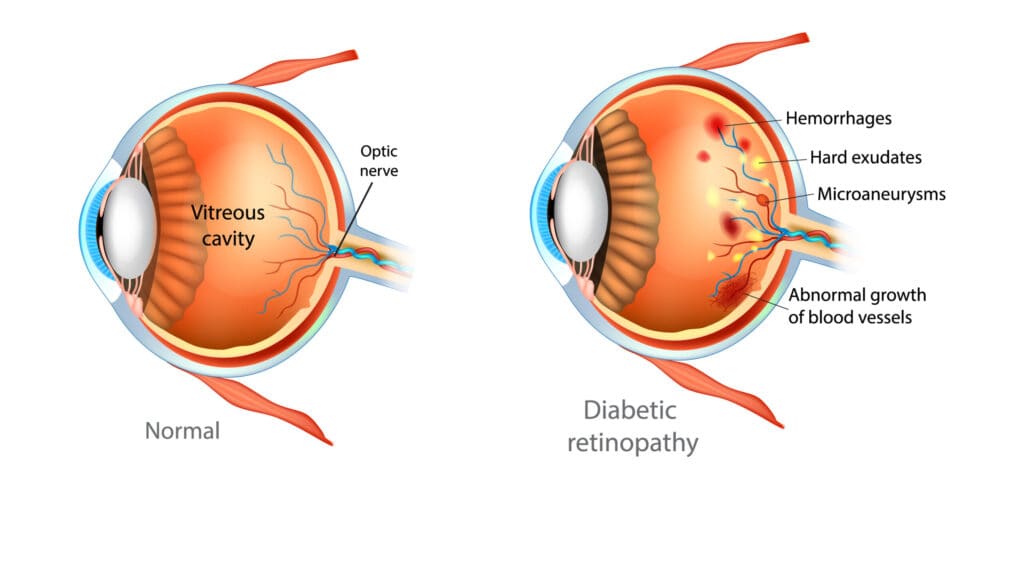
The main cause of diabetic retinopathy is high blood sugar due to diabetes, which damages blood vessels throughout the body.
Excess sugar blocks the small blood vessels that supply your retina, leading to fluid leakage and bleeding.
Your eyes respond by growing new blood vessels that are not effective and can also leak or bleed.
Diabetic retinopathy symptoms
In the early stages of diabetic retinopathy, you might not have any symptoms.
However, you may notice changes in your vision, such as difficulty reading or seeing faraway objects, that come and go.
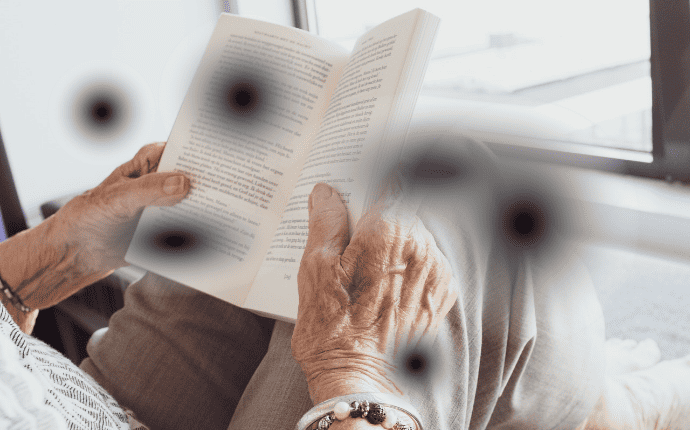
As the disease progresses, the blood vessels in your retina may start to bleed into the fluid that fills your eye (vitreous).
Leakage and bleeding inside your eye may cause you to see dark, floating spots or streaks that look like cobwebs.
Sometimes, these spots may clear up on their own, but you should seek treatment immediately.
Without treatment, scars may form in the back of your eye, and the blood vessels may start to bleed again or worsen the bleeding.
Diabetic retinopathy diagnosis
If you have diabetes, it’s important that you get regular eye exams to check for diabetic retinopathy.
Your opthalmologist will perform a simple and painless dilated eye exam, where they will give you eye drops to widen your pupil and check for any problems with your retina.
During the exam, your doctor may also perform additional tests, such as:
- Visual acuity test
- Visual field test
- Eye muscle function test
- Pupil response test
- Tonometry test
The visual acuity test is used to assess how clearly you see, and your eye specialist will ask you to read letters up close and far away.
The visual field test checks your peripheral vision, testing how well you can see objects off to the sides without moving your eyes.
Your ophthalmologist will also perform an eye muscle function test, where they will move an object around and evaluate how well you follow it with your eyes.
The pupil response test is used to check how light enters your eyes.
The tonometry test will measure the pressure in your eyes or intraocular pressure (IOP).
Finally, your ophthalmologist will perform dilation to check for any issues with the inner parts of your eye.
They will give you some eye drops to widen your pupil, which helps them see inside your eye.
If your eye specialist suspects severe diabetic retinopathy or DME, they may also perform a fluorescein angiogram to see pictures of the blood vessels in your retina.
Remember that early treatment for diabetic retinopathy can help prevent vision loss.
Diabetic retinopathy treatment
Diabetic retinopathy treatment cannot reverse any vision loss, but it can stop it from getting worse.
If you’ve been diagnosed with diabetic retinopathy, your eye specialist may monitor your eyes closely in the early stages to track their progress.
You may need a comprehensive dilated eye exam as often as every 2 to 4 months.
It’s particularly important that you manage your diabetes, blood pressure, and cholesterol levels.
If you experience changes in your vision, it’s important to start treatment right away.
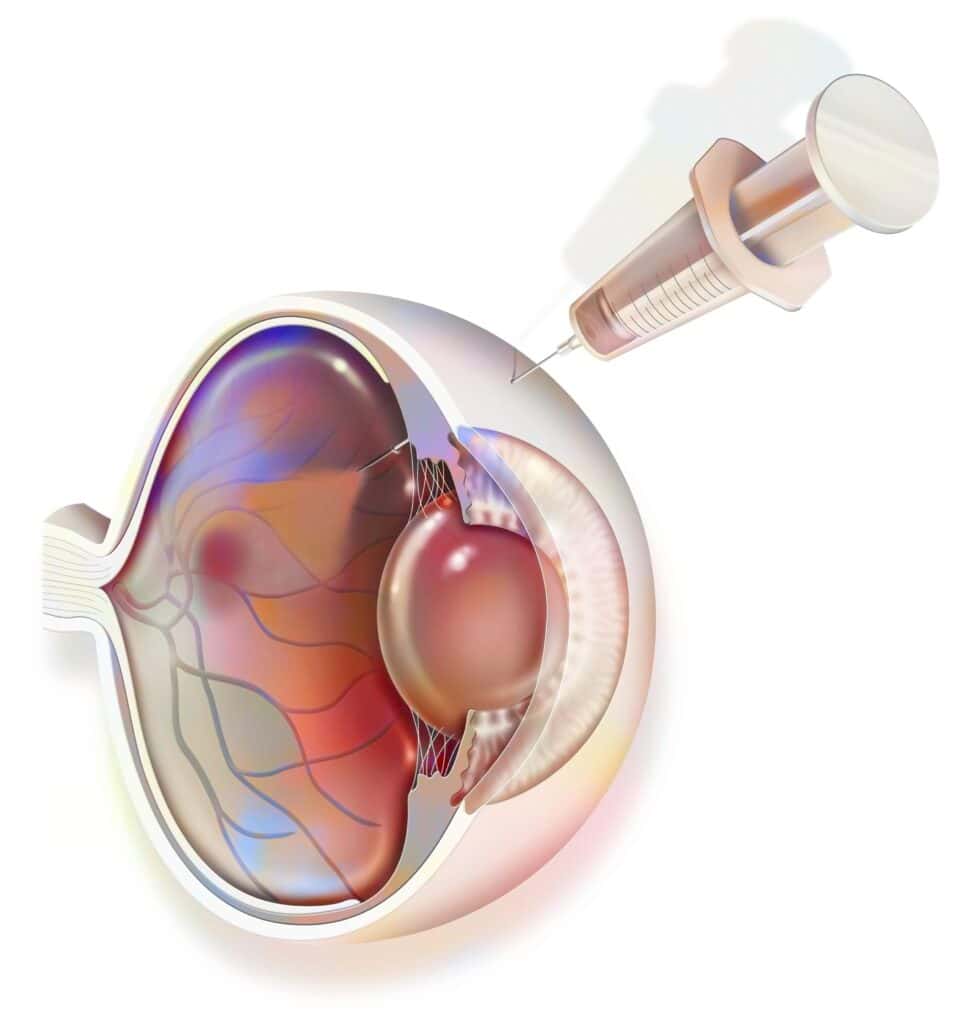
To slow down or reverse diabetic retinopathy, you may receive injections of anti-VEGF drugs, which can be effective in blocking a protein called vascular endothelial growth factor (VEGF).
Corticosteroids can also be used alone or in combination with other treatments to suppress DME, although they increase the risk of cataracts and glaucoma, and are not the treatment of choice.
Anti-VEGF injection therapy or focal/grid macular laser surgery may be effective in treating diabetic macular edema.
Your ophthalmologist may also recommend laser treatment to reduce swelling in the retina, by shrinking and stopping leaking blood vessels.
Eye surgery, such as a vitrectomy, may be an option if there is significant bleeding in your retina or a lot of scars in your eye.
Vitrectomy is the surgical removal of the vitreous gel in the center of the eye to treat severe bleeding into the vitreous.
For proliferative diabetic retinopathy (PDR), scatter laser surgery is a common treatment, along with anti-VEGF injections.
Why choose Vision Pros to treat your diabetic retinopathy?
- Experienced ophthalmology team with expertise in all areas of ophthalmology, optometry, and general eye care.
- Rapid access and referral to world-class comprehensive screening and cutting-edge treatment in a state-of-the-art ophthalmology clinic.
- Holistic, personal, and patient-centric approach to every aspect of eye care.
Book an appointment for your comprehensive eye examination today
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
- https://www.nei.nih.gov/sites/default/files/health-pdfs/Diabetic_Retinopathy_What_You_Should_Know.pdf
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy/laser-treatment-diabetic-retinopathy
- https://www.nei.nih.gov/learn-about-eye-health/healthy-vision/get-dilated-eye-exam