Conditions
Posterior vitreous detachment
Posterior vitreous detachment is a form of retinal detachment that commonly affects people as they age, resulting in a range of vision problems.
What is posterior vitreous detachment (PVD)?
Posterior vitreous detachment, or PVD for short, is a vitreous-related disease that is commonly associated with old age.
As you get older, the posterior vitreous–the gel-like substance at the back of your eye–degenerates and separates or detaches from the retinal layer.
As the vitreous thins and liquefies, it can no longer fill the ocular cavity (the inside of your eye) and pulls away from the retina.
The tration on the retina may lead to a break in the tissues which can progress to a retinal detachment.
Retinal detachment may impair your vision and cause permanent blindness if left untreated.


What causes posterior vitreous detachment?
PVD is a very common condition, that is to a certain degree, a normal part of the natural history of aging of the human eye.
The causes and risk factors associated with posterior vitreous detachment (PVD) increase as you age.
You’re more at risk of PVD if you experience one or more of the following:
- Myopia (nearsightedness)
- Trauma to the eye
- Eye surgery
- Eye injections
- Uveitis
- Family history
- Certain medical conditions such as Stickler Syndrome
- Diabetes
If you’ve been diagnosed with posterior vitreous detachment in one eye, you’re more likely to experience PVD in the other eye within a year of the first diagnosis.
Posterior vitreous detachment symptoms
Most cases of posterior vitreous detachment commonly present with floaters, with or without flashes, but don’t result in visual loss per se, although about 10% of patients with PVD are at risk to develop retinal detachments which is vision threatening, and is a medical emergency.
One of the most common symptoms of this benign form of PVD is floaters, which don’t necessarily impair your vision.
Floaters are blurry dark spots that may be annoying but usually subside over time.
However, if you experience extensive floaters along with flashes of light appearing in your peripheral vision, you may be diagnosed with PVD that’s complicated by a retinal tear or bleeding inside the eye (vitreous hemorrhage).
As posterior vitreous detachment progresses, you may experience an increased number of floaters and flashes as well as distorted vision.

Posterior vitreous detachment diagnosis
Posterior vitreous detachment is typically diagnosed with a dilated eye exam, an optical coherence tomography (OCT), or an ocular ultrasound.
Additional diagnosis methods for PVD include slit-lamp biomicroscopy and B-scan ultrasonography.
- Dilated eye exam
- Optical coherence tomography (OCT)
- Slit-lamp biomicroscopy
- Ocular ultrasound

Dilated eye exam
During a dilated eye exam, the ophthalmologist will apply drops to your eye to dilate or widen the pupil.
They will then shine light into your eye to observe the retina and identify any retinal tear or signs of PVD.
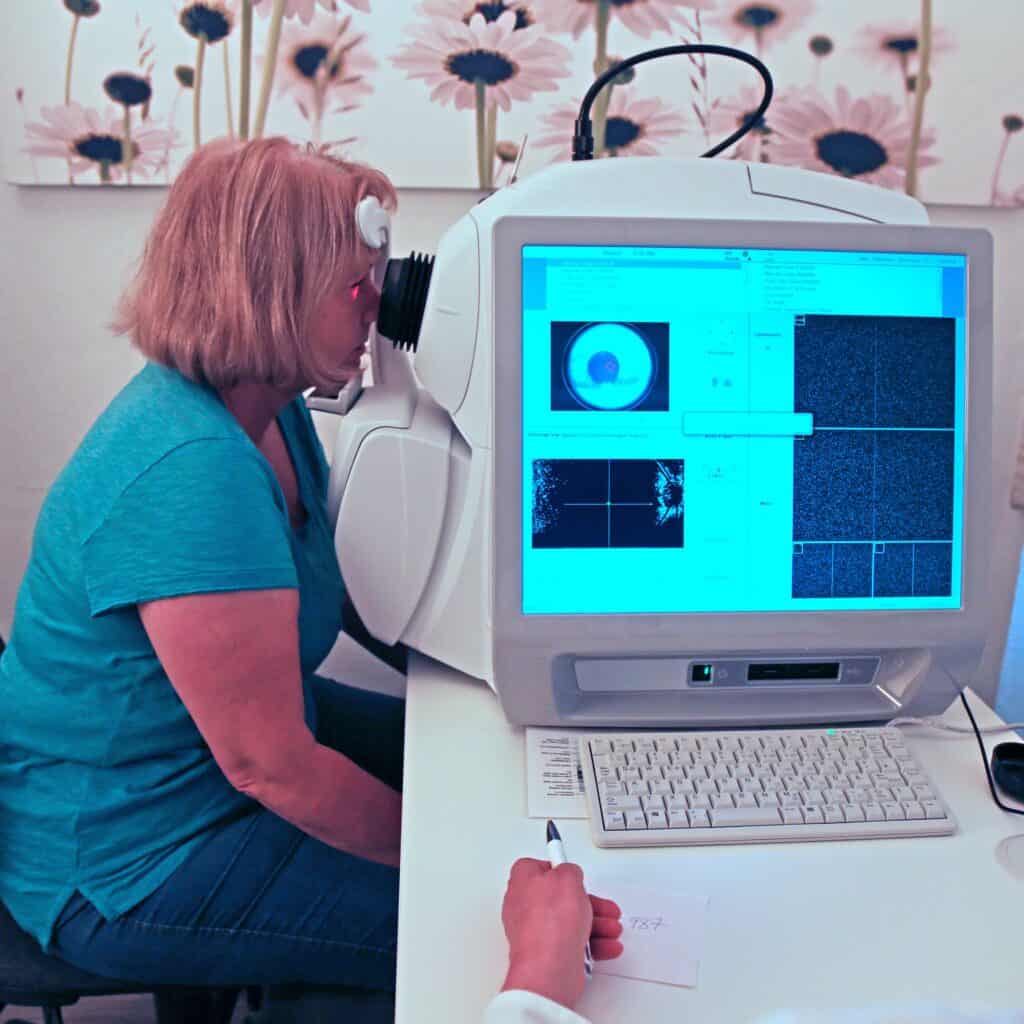
Optical coherence tomography (OCT)
Optical coherence tomography (OCT) is a non-invasive ocular imaging tool that helps your ophthalmologist see inside your eye and evaluate the retina and vitreous.
OCT can identify early signs of posterior vitreous detachment better than tests like slit-lamp biomicroscopy or B-scan ultrasonography.

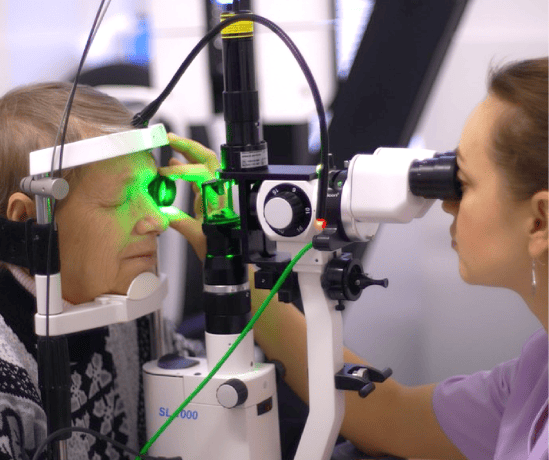
Slit-lamp biomicroscopy
Slit-lamp biomicroscopy involves the use of medications called mydriatic agents that fully dilate your pupils so that the ophthalmologist can observe as much of the vitreous as possible.
Slit-lamp biomicroscopy allows your eye specialist to identify whether the posterior vitreous detachment is
- Complete (C-PVD)
- Partial (P-PVD)
- Collapsed
- Without a collapse

Ocular ultrasound
Ocular ultrasound is a painless diagnostic test that uses high-frequency waves to create an image of the inside of your eye and identify signs of PVD.
This procedure is also known as B-scan ultrasonography, ocular echography, echo, or ultrasonography (US).
Posterior vitreous detachment treatment
The initial symptoms of posterior vitreous detachment–floaters and flashes–usually disappear within three months of diagnosis.
Your ophthalmologist may recommend that you have another dilated eye exam 4-6 weeks after the initial diagnosis to rule out the development of retinal tears or detachments.
In the absence of any damage to the retina, no treatment is required. Observation is recommended, patients are explained to consult rapidly if they note any increase of floaters, start or increase in flashes, and/or loss of vision or visual field defect,
If a patient has a retinal tear they will be offered emergency a very safe and vision saving laser treatment, promptly performed at Vision Pros by one of our competent Ophthalmologists, called laser retinopexy.
If a patient has a retinal detachment, they will be rapidly sent to one of our Surgical Retina colleagues in the hospital system to perform vision saving surgery. A variety of techniques may be employed:
- Pneumatic retinopexy
- Scleral buckle
- Vitrectomy
- Silicone oil
Why choose Vision Pros to treat your posterior vitreous detachment?
- Experienced ophthalmology team of specialists with expertise in all areas of ophthalmology, optometry, and general eye care.
- Rapid access and referral to world-class comprehensive screening and cutting-edge treatment in a state-of-the-art ophthalmology clinic.
- Holistic, personal, and patient-centric approach to every aspect of eye care.
Book an appointment for your comprehensive eye examination today
- https://www.asrs.org/patients/retinal-diseases/9/posterior-vitreous-detachment
- https://www.aao.org/eye-health/diseases/what-is-posterior-vitreous-detachment
- https://www.ncbi.nlm.nih.gov/books/NBK563273/
- https://www.webmd.com/eye-health/posterior-vitreous-detachment-facts
- https://eyerounds.org/tutorials/ultrasound/index.htm