Conditions
Cataracts
Get an appointment with an ophthalmologist to treat your cataracts in as quickly as one week. No referral needed.
Cataracts are one of the “big five” eye diseases identified as the main causes of vision loss, along with glaucoma, age-related macular degeneration, diabetic retinopathy, and eye injuries.
What are cataracts?
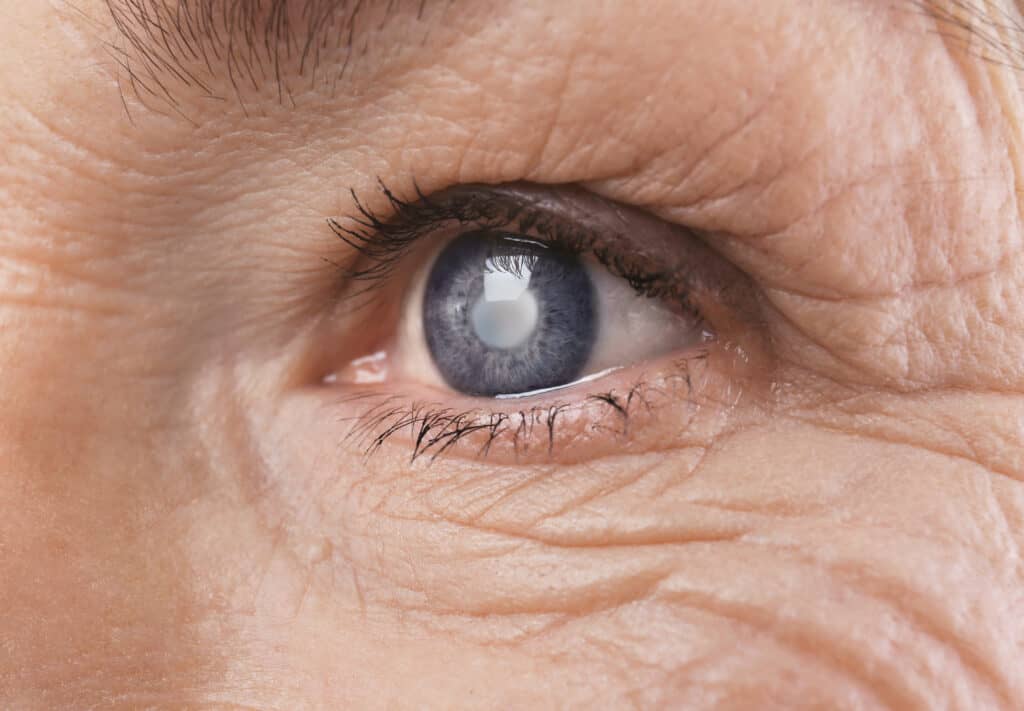
Cataracts are a clouding or thickening of the crystalline lens, which resides in the pupil, right behind the iris. They can be of slow or more rapid onset, but generally speaking, cataracts develop over time, and are much more common as we age.
In some cases, children and even babies can develop cataracts, and rarely, children can be born with them.
There are 4 main types of cataracts:
- Nuclear cataracts
- Cortical cataracts
- Posterior subcapsular cataracts
- Congenital cataracts
Nuclear cataracts
Nuclear cataracts affect the center of the lens in your eye.
Over time, the lens turns yellow and cloudy, reducing your vision.
Nuclear cataracts may cause an inability to distinguish between different shades of color.
Cortical cataracts
Cortical cataracts can lead to vision loss as well, and patients may become symptomatic with glare and halos at night as a first symptom, but this holds true for all cataracts.
Posterior subcapsular cataracts
Posterior subcapsular cataracts affect the back of the lens in your eye, and typically progress faster than nuclear or cortical cataracts.
Posterior subcapsular cataracts affect your ability to read and see in bright light conditions.
You may also experience glare at night or in low-light conditions.
Congenital cataracts
Congenital cataracts appear at birth and may be genetic or caused by trauma or an intrauterine infection during pregnancy.
Other causes of congenital cataracts include, but are not limited to, the following:
- Myotonic dystrophy
- Galactosemia
- Neurofibromatosis type 2
- Rubella
What causes cataracts?
The vast majority of cataracts are age related, and likely represent a normal aging process of the crystalline lens, but they can also be related to trauma, UV exposure or other risk factors, certain medical conditions, and genetics
This change in the lens is typically the result of proteins lens material breaking down and clouding your vision, in a variety of ways:
Some of the risk factors associated with cataracts include the following conditions or health problems:
- Eye surgery
- Diabetes
- Steroid medications
- Smoking
- High blood pressure
- Excessive alcohol consumption
- Exposure to excessively bright light
- Obesity
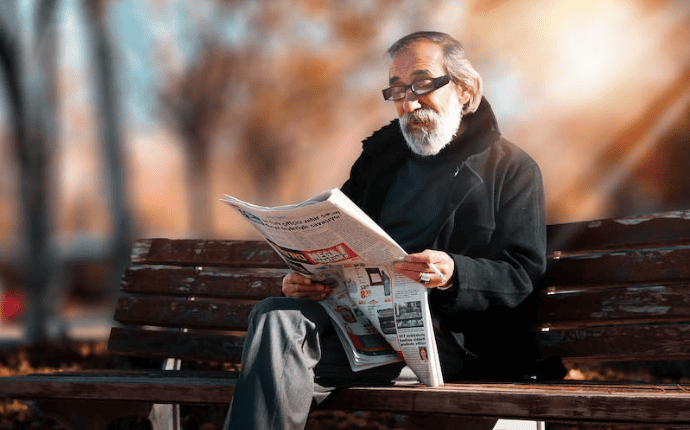
Cataracts symptoms
The symptoms of cataracts are usually painless and include one or more of the following:
- Cloudy or blurred vision
- Dull vision
- Reduced or impaired vision in low-light conditions
- Light sensitivity
- Glare or halos around light at night
- Double vision in one eye
Cataracts diagnosis
Your ophthalmologist may diagnose cataracts in one or both eyes by identifying the symptoms listed above and performing a comprehensive eye examination.
An eye exam to diagnose cataracts includes:
- A visual acuity test
- A slit-lamp examination
- Tonometry (pressure)
- Full retinal exam
- OCT to rule out Glaucoma and Macular pathologies
- Biometry
- Corneal topography

Visual acuity exam
A visual acuity exam is an eye chart test used to assess your vision from various distances.
Your ophthalmologist will combine the results of the Amsler grid test and a visual acuity exam to diagnose AMD more accurately.

Retinal exam
Your ophthalmologist will perform a retinal exam by first applying eye drops to dilate or widen your pupils so they can easily see the optic nerve at the back of your eyes using a slit-lamp.

Slit-lamp examination
During a slit-lamp examination, your ophthalmologist will use a very bright, focused light to see the inside of your eye and examine your cornea, iris, and lens for any damage.
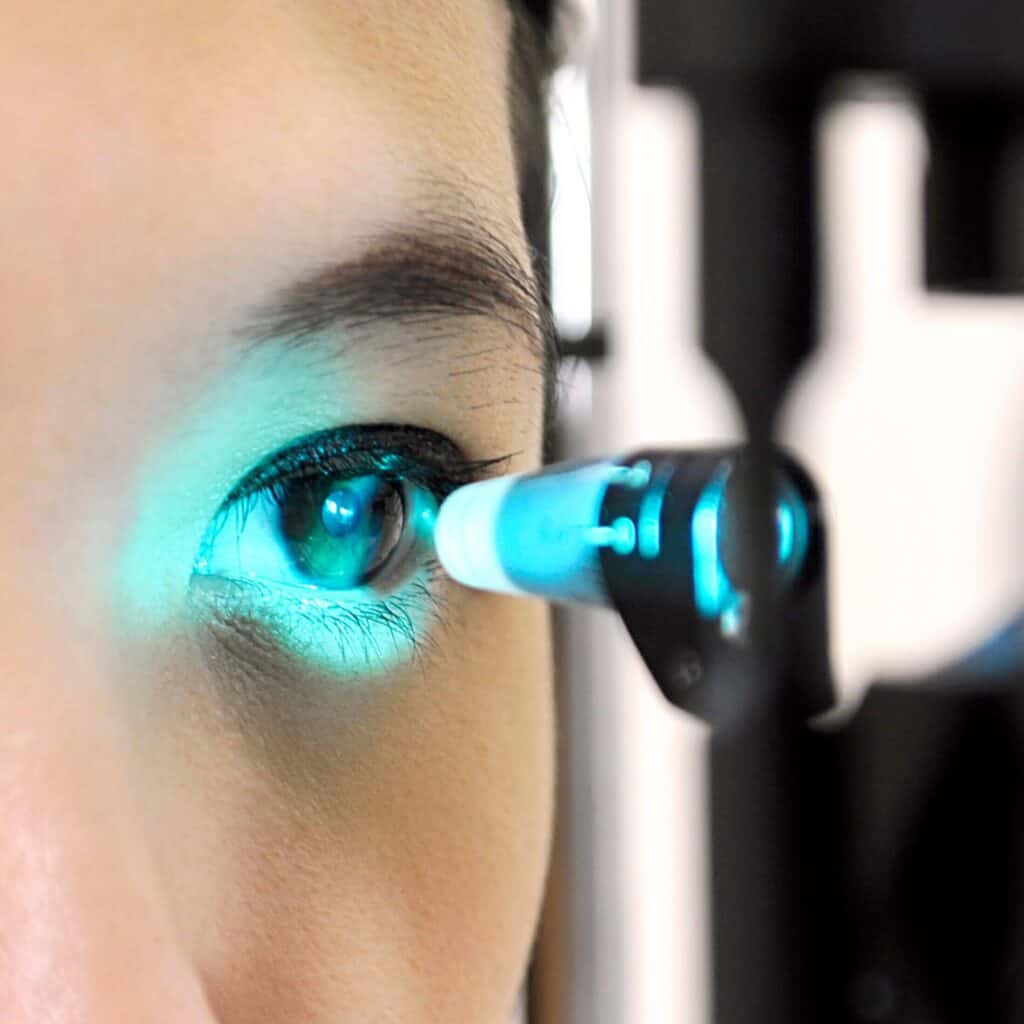
Tonometry
An applanation tonometry is a test that helps your ophthalmologist measure the intraocular pressure (IOP) inside your eye.
A high IOP may indicate other conditions, such as glaucoma.

Cataracts treatment
Cataracts may be observed when in the mild stage, and vision can often be improved with glasses or even contact lenses.
As your vision becomes impaired, your eye specialist may recommend cataract surgery, also known as phaco-refractive surgery.
Phaco-refractive surgery involves the removal of the cloudy, yellowing lens inside your eye.
The damaged lens is then replaced with any of the following intraocular lenses (IOLs), which aim to correct your vision:
- Monofocal lenses
- Multifocal or trifocal lenses
- Extended depth-of-field (EDOF) lenses
- Toric lenses for astigmatic correction
Why choose Vision Pros to treat your cataracts?
- Experienced ophthalmology team of specialists with expertise in all areas of ophthalmology, optometry, and general eye care.
- Rapid access and referral to world-class comprehensive screening and cutting-edge treatment in a state-of-the-art ophthalmology clinic.
- Holistic, personal, and patient-centric approach to every aspect of eye care.
Book an appointment for your comprehensive eye examination today
- https://www.cos-sco.ca/report-provides-20-20-vision-on-value-of-ophthalmology-in-canada/
- https://www.mayoclinic.org/diseases-conditions/cataracts/symptoms-causes/syc-20353790
- https://www.aao.org/eye-health/diseases/what-are-cataracts
- https://my.clevelandclinic.org/health/diseases/8589-cataracts
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/cataracts
- https://www.healthdirect.gov.au/cataracts
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/cataracts#:~:text=What%20are%20cataracts%3F,to%20get%20rid%20of%20cataracts.
- https://youtu.be/D7lONeb3ONI
- https://youtu.be/u_l0rY_Z-pE
- https://youtu.be/3sjtN6tratU
- https://youtu.be/BmhwqYDDYgQ
- https://youtu.be/FSgRFpYQ638
- https://youtu.be/TqR-WlH2ROM
- https://david-richardson-md.com/lp/cataract-surgery-using-laser-is-it-really-worth-the-high-cost/
- https://cliniquebellevue.com/en/phacorefractive-surgery-a-flexible-solution/
- https://youtu.be/VPKDse027AA